Epilepsy — The Invisible Disability
Epilepsy is often misunderstood because most of its challenges happen out of sight. While seizures are the most recognized symptom, the real impact extends far beyond, from fatigue and medication side effects to anxiety, memory lapses, and the constant fear of judgment. Epilepsy is an invisible disability and those living with it are often misunderstood simply because they “look fine.” It’s a disability that shapes daily life in ways others rarely see. People may appear healthy, but behind that normalcy lies constant vigilance, adjustment, and resilience. This article explores what living with epilepsy truly means, breaking through common misconceptions and highlighting why awareness, empathy, and informed support are essential to improving lives.
Dr. Clotilda Chinyanya
11/7/20254 min read
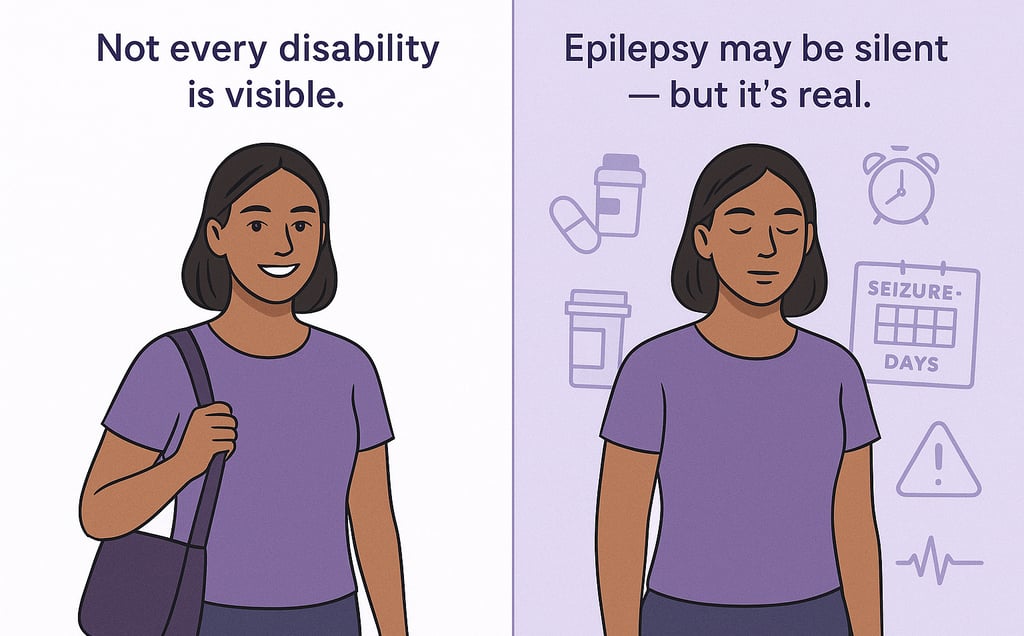
When people think of disability, they often picture something visible: a wheelchair, a walking aid, or someone who is obviously unwell. But millions of people live with conditions that are rarely seen yet deeply felt. These are called invisible disabilities, and epilepsy is one of the most misunderstood among them. Epilepsy is not always on display. It doesn’t announce itself constantly. It can stay quiet for days, weeks, or even years, but that doesn’t make it any less real. Living with it is often like carrying an unpredictable storm inside your brain. There may be calm skies for a while, but at any moment, thunder could strike. That silent unpredictability is what makes epilepsy both invisible and exhausting.
What Makes Epilepsy “Invisible”?
The invisibility of epilepsy lies not only in the fact that seizures aren’t constant, it's also in how the impact lingers long after a seizure ends.
People living with epilepsy often look perfectly healthy most of the time. They go to work, socialize, raise families, and live full lives. But what isn’t seen is:
The constant risk calculation - “What if I have a seizure here?” “Should I sit near an exit?” “Can I take this bus alone?”
The silent symptoms between seizures - brain fog, headaches, dizziness, and memory lapses caused by medication or brain activity
The strict routines - medication must be taken at precise times, sleep schedules must be consistent, alcohol or stress must be carefully controlled
Even when seizures aren’t happening, epilepsy never fully leaves. The brain is in a constant state of management mode.
And unlike visible disabilities, epilepsy comes with no physical warning signs. There’s no brace or badge that says “I may need help unexpectedly.” Someone may be laughing with friends one moment and unconscious on the floor the next and no one saw it coming. This unpredictability makes epilepsy not only invisible, but often misunderstood.
The Hidden Impact on Daily Life
Even between seizures, epilepsy shapes choices that others take for granted. People living with it are constantly balancing independence with safety.
Everyday Activities and Hidden Complications
Driving: Many countries require a seizure-free period (from 6 months to 2 years) before issuing or renewing a license. Losing driving rights can cost someone their job or independence.
Career Choices: Roles involving heights, heavy machinery, or night shifts may be restricted. Some employers quietly avoid hiring people with epilepsy due to liability fears.
Education: Medication side effects can make concentration and memory difficult, yet students may be labelled “lazy” or “unfocused”.
Friendships & Social Life: Fear of having a seizure in public makes many self-isolate. Invitations get declined not because they don’t care, but because they don’t feel safe.
Living with epilepsy often means living with invisible caution.
When Invisibility Leads to Misunderstanding
Because epilepsy isn’t always obvious, others sometimes downplay it.
“You don’t look sick.”
“But you were fine yesterday.”
“Is it really that serious?”
These statements, while usually well-intentioned, can feel dismissive. They suggest that the condition only matters when a seizure happens, as if the rest of the struggle doesn’t count.
Some people with epilepsy even report being accused of “faking” or “overreacting” because, on the outside, they seem well. Others face pressure to stop taking medication because “you look cured now.”
Invisibility can also lead to unsafe assumptions in emergencies. Many bystanders freeze or panic when witnessing a seizure, not because they don’t care, but because they didn’t know the person had epilepsy. If they had known beforehand, they might have been able to help confidently.
The irony is striking:
People hide their condition to avoid stigma, but hiding it can put them at risk when they need support the most.
Stigma Still Exists Even Today
Medical science has progressed, but public perception hasn’t always kept up.
In some parts of the world, epilepsy is still surrounded by superstition. People have been:
Denied education because seizures were seen as “possession”
Forced into isolation or institutionalization
Refused marriage because families believed epilepsy was “contagious”
Fired after a single public seizure
Even in modern countries, stigma exists in more subtle ways:
Employers quietly choose another candidate.
Highly qualified people are under-employed.
Friends stop inviting someone after witnessing a seizure.
Teachers suggest “simpler goals” for a student with epilepsy.
Strangers record seizures instead of helping, mistaking them for “odd behavior” or intoxication.
It’s not always cruelty. Often, it’s ignorance.
But ignorance can hurt just as much as discrimination. This is why visibility and awareness are not optional — they’re urgent.
How You Can Support Someone with Epilepsy (Even If You Never See Their Seizures)
You don’t need medical training to be an ally. You only need awareness and empathy.
✅ Believe them. If someone says they are struggling, even if they look fine, take them seriously.
✅ Learn seizure first aid. Stay calm, cushion their head, time the seizure, and never put anything in their mouth.
✅ Respect boundaries. Some people want to talk openly, others prefer privacy, let them lead.
✅ Advocate for inclusion. Schools, workplaces, and public spaces should be seizure-safe and welcoming.
✅ Challenge stigma when you hear it. A simple, “Actually, that’s not how epilepsy works,” can change a conversation.
Why Visibility Matters
Epilepsy may be invisible, but its effects aren’t. Acknowledging it as a disability even when symptoms aren’t visible means:
People get the accommodations they need instead of being dismissed.
Emergency responses are faster and safer when others know what’s happening.
Isolation turns into community when people feel safe to speak openly.
The more we normalize discussions around epilepsy, the less people will feel the need to hide it.
Final Thought: You Don’t Have to See a Disability to Respect It
Epilepsy doesn’t always shout. Sometimes it whispers. It hides in quiet exhaustion, medication alarms, cautious decisions, and unspoken fears.
But just because something isn’t seen doesn’t mean it isn’t lived.
If we listen without judgement, we make room for dignity, safety, and understanding.
Support should never depend on what the eye can see.
Epilepsy may be invisible but the people living with it shouldn’t be. See them.
Be informed.