Understanding Focal Autonomic Seizures: Meet Joyce
Focal autonomic seizures are one of the most misunderstood seizure types because they don’t always look like seizures. Instead of dramatic convulsions, they often present as sudden changes in heart rate, breathing, digestion, skin color, or bladder sensations, experiences that feel intensely physical and deeply unsettling. Many people are misdiagnosed for years with anxiety, panic attacks, gastrointestinal illness, or heart problems before epilepsy is considered. This blog post explains focal autonomic seizures in clear, human terms, grounding the science in real-life experience. Through the story of Joyce, you’ll see how these seizures feel from the inside, why they happen, how they’re diagnosed, and what treatment and support can look like.
Dr. Clotilda Chinyanya
11/30/20254 min read
Joyce’s Story: “Something Is Wrong with My Body”
Joyce was used to listening to her body. As a graphic designer, she spent long hours at her desk, so she knew the difference between hunger and stress, between a skipped meal and a bad night’s sleep. That’s why the first episode unsettled her so deeply.
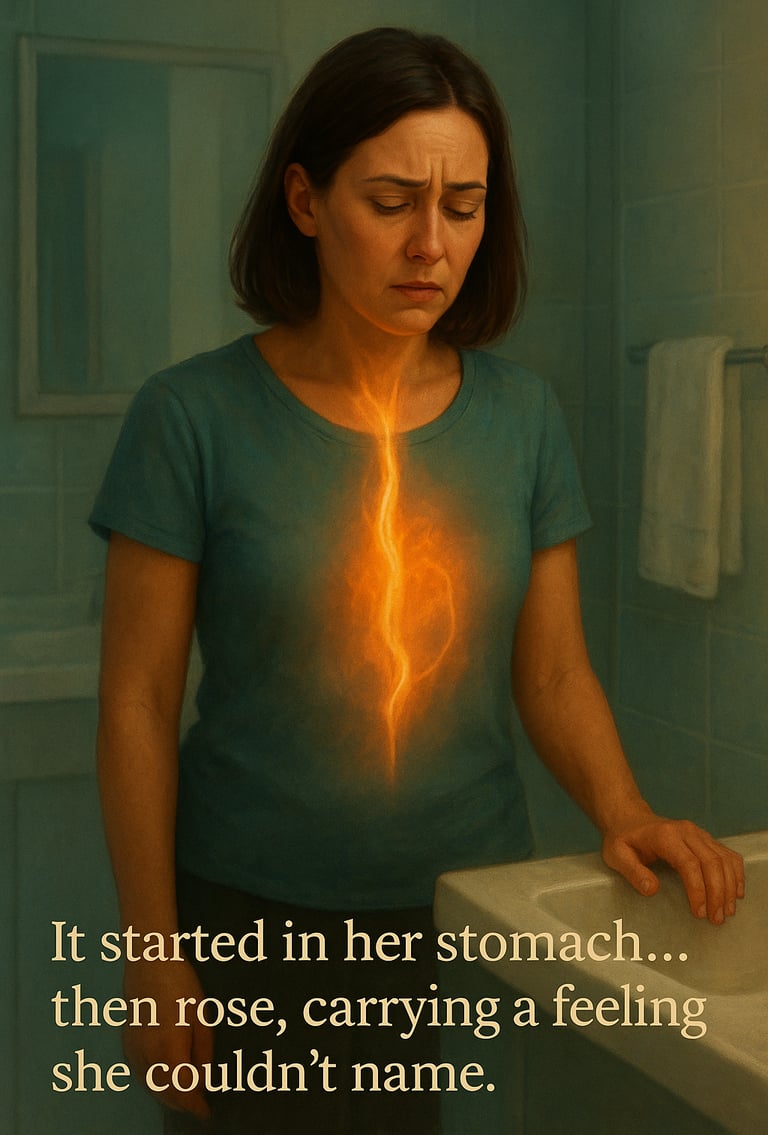
It started one morning while she was brushing her teeth. Out of nowhere, a strange sensation bloomed in her upper abdomen, like a tight knot twisting inward. Then it began to rise, slowly and deliberately, climbing from her stomach into her chest and throat. Her heart suddenly started racing, pounding so loudly she was sure she could hear it echo in her ears. Her face felt hot, then icy cold. A wave of nausea followed, and with it an overwhelming certainty: Something is wrong.
She leaned against the sink, breathing fast, then slower, then not quite sure how to breathe at all. The episode lasted maybe a minute. When it passed, Joyce was left shaky, exhausted, and confused but fully awake the entire time.
Her doctor suggested anxiety. Another wondered about acid reflux. A cardiologist ordered heart tests, all of which came back normal. The episodes kept happening. Sometimes they came with an urgent need to use the bathroom. Sometimes her skin prickled with goosebumps, even in a warm room. Once, while grocery shopping, she suddenly felt dizzy and pale, her heart slowing instead of speeding up, as if it might stop altogether. She never lost consciousness, but she felt as though her body was briefly no longer under her control.
The most frightening part wasn’t the symptoms themselves, but the unpredictability. Joyce began to fear everyday moments: standing in line, driving, even laughing too hard. She wondered if she was “missing something obvious” or if it was all in her head. It wasn’t.
After one episode was captured during prolonged video-EEG monitoring, a neurologist finally named what Joyce was experiencing: focal autonomic seizures, arising from deep structures in her temporal lobe. For the first time, Joyce felt relief, not because the seizures were gone, but because her experience finally made sense and there was hope.
What Are Focal Autonomic Seizures?
Focal autonomic seizures are focal-onset, non-motor seizures that begin in one area of the brain and primarily affect the autonomic nervous system, the system responsible for involuntary functions like heart rate, blood pressure, digestion, breathing, sweating, and bladder control.
To be classified as a focal autonomic seizure, autonomic symptoms must be present at the very onset of the seizure. If autonomic symptoms appear later, they are described as seizure features rather than the defining onset.
These seizures may occur:
With retained awareness (often experienced as an “aura”)
With impaired awareness
Or as the initial phase before spreading into another seizure type, including focal impaired awareness seizures or focal-to-bilateral tonic-clonic seizures
Why They’re Often Missed
Because focal autonomic seizures don’t always involve visible movements, they are frequently mistaken for:
Panic attacks
Gastrointestinal disorders
Migraines
Heart rhythm problems
Hormonal or stress-related conditions
Like Joyce, many people spend years searching for answers outside neurology.
The Central Autonomic Network: Where These Seizures Begin
Focal autonomic seizures arise from disruption of the central autonomic network (CAN), a distributed system of brain regions that regulate involuntary bodily functions. Key components include:
The insula, often described as the brain’s primary viscerosensory cortex
The amygdala and mesial temporal structures
The medial prefrontal cortex
The hypothalamus
Brainstem centers that control breathing, heart rate, and blood pressure
When an epileptic discharge activates this network, the body may abruptly shift into a sympathetic (“fight-or-flight”) or parasympathetic (“rest-and-digest”) state, or oscillate unpredictably between the two. This explains why symptoms can feel intense, sudden, and deeply physical.
Common Symptoms of Focal Autonomic Seizures
Focal autonomic seizures are remarkably diverse. Symptoms can be subjective (felt by the person), objective (observed by others), or both.
Cardiovascular Symptoms
Rapid heart rate (tachycardia)
Slow heart rate (bradycardia)
Irregular rhythms
Paleness or flushing
In rare cases, ictal asystole, which may cause collapse or convulsive movements due to reduced blood flow to the brain
Gastrointestinal Symptoms
Epigastric sensations (tightness, churning, emptiness, rising feeling)
Nausea or vomiting
Abdominal pain or discomfort
Urgent hunger or fullness
The classic “rising” sensation from the stomach to the throat, experienced by Joyce, is one of the most recognized autonomic auras.
Respiratory Symptoms
Shortness of breath
Hyperventilation or slowed breathing
Choking or coughing
Apnea (temporary stopping of breathing)
Respiratory involvement is clinically important, as it may contribute to serious complications when prolonged.
Skin and Temperature Changes
Sweating
Goosebumps (piloerection)
Sudden warmth or cold
Pallor or flushing
Pupillary Changes
Dilated or constricted pupils
Reduced responsiveness to light
Urinary and Sexual Symptoms
Sudden urge to urinate or defecate
Urinary incontinence in some cases
Genital sensations, erection, or orgasm (rare but documented)
Awareness and Aftereffects
Awareness during focal autonomic seizures varies. Many people remain fully aware, which can make the experience especially frightening. Others develop confusion or impaired awareness as the seizure progresses. After the seizure, individuals may experience:
Fatigue
Headache
Emotional distress
Confusion or disorientation
Fear of recurrence
Joyce described the aftermath as “feeling like my nervous system had just run a marathon.”
Diagnosis: Putting the Puzzle Together
Diagnosing focal autonomic seizures often requires persistence. Key elements include:
Detailed history, especially first symptoms and sequence
Video-EEG monitoring, sometimes prolonged
Cardiac and respiratory monitoring during seizures
Neuroimaging, such as MRI, to evaluate underlying brain structures
Because symptoms can mimic other conditions, capturing an episode during EEG is often crucial.
Treatment and Management
Treatment is individualized and may include:
Anti-seizure medications (anti-epilepsy drugs) to reduce seizure frequency and severity
Lifestyle adjustments, such as improving sleep, hydration, and stress management
Addressing seizure triggers, when identifiable
Advanced therapies, including surgical or neuromodulation options, in selected cases
The goal is not only seizure control, but restoring confidence in daily life, something Joyce slowly began to regain once her seizures were understood and treated.
Living with Focal Autonomic Seizures
Focal autonomic seizures remind us that epilepsy is not just a disorder of movement or consciousness, it is also a disorder of the body’s most fundamental regulatory systems. For Joyce, the diagnosis didn’t erase fear overnight, but it gave her language, validation, and a path forward. She learned to recognize her early warning signs, advocate for herself, and explain her condition to others without shame.
And perhaps most importantly, she learned this truth:
Just because a seizure doesn’t look dramatic doesn’t mean it isn’t real.
Summary
Focal autonomic seizures:
Begin in one hemisphere of the brain
Present with autonomic symptoms at onset
Can occur with or without impaired awareness
Are commonly misdiagnosed
Reflect disruption of the central autonomic network
Understanding them requires listening carefully to both neuroscience and lived experience. When we do, stories like Joyce’s move from confusion to clarity, and from fear to informed care.
Further Reading:
Choose Knowledge: